You may be wondering if you are hypothyroid or know of someone who is. There’s a current upsurge in interest in this subject and using diet and lifestyle to help balance this condition. I was diagnosed over ten years ago. Typically the MD’s will check your TSH (thyroid-stimulating hormone) and if that’s within a given range, they’ll stop there and tell you your thyroid is fine. When I was increasingly tired, the MD I was going to at the time suggested checking my thyroid. She said if it’s your thyroid, no problem, you start on Synthroid® (brand name for levothyroxine) and you’re good to go—simple solution. She made it sound like it was quite common. “Take a pill and you’re done.” (Sadly it IS quite common. Synthroid® is the most prescribed medication in the US.–as of the time of this post. That has since changed as I update this in 2023. It’s currently Lipitor. Reac on to see the part about cholesterol.)
Over the past 10+ years I’ve painstakingly discovered many things about hypothyroidism. What I’m about to share is my own research and my own decisions made for myself. The list is NOT exhaustive, I’m sure. They’re not meant to be your blueprint or to make your decisions so much as for you to be aware of areas you might want to research for yourself. This is my way of saying I don’t even play a doctor on TV! So do your research and talk to your doctor!
Here’s what I wish the MD would have done and/or told me at the time of diagnosis:
~~
- Hypothyroid disease is associated with diabetes (the pancreas is part of the endocrine system) and increases your chances of other auto-immune diseases (the thymus governs the immune system and is part of the endocrine system. You’re taking blood to check my thyroid which is part of the endocrine system. Why not check out the other family of organs in that system? They all work together. I’d had more than one blow to the head over my lifetime (childhood falls, line-drive to the head during softball requiring eight stitches, neck/back injury almost 20 years ago now.) Traumatic brain injury can injure your pituitary gland (another endocrine gland) and even years later can be associated with hypothyroid disease, adrenal insufficiency, diabetes…there’s more.
It took me well over eight years to decide to switch doctors over another matter—my regular doctor left the practice and the new one thought my “outie” bellybutton was a hernia! This was after she asked why in the world I’d want to check my vitamin D levels? (Inside I was thinking—what rock have you been under and where did you go to medical school? I’m always reading how little nutrition education MDs receive, but by this time Vitamin D’s importance had gone mainstream. Mental note to self, this doctor is dangerous to my health.)
~~
- Vitamin D is a hormone and low levels are associated with a higher risk of thyroid antibodies which are found with autoimmune thyroid disorders like Hashimotos Disease. Yup that’s right and I have discovered that low levels affect many bodily functions. I didn’t know this particular detail of Vitamin D at the time. I just knew it was an uber-important vitamin (can you say cancer risk and progression for starters?) and living in Minnesota increased my odds of being low on Vitamin D since we make very little Vitamin D except during the summer and sun screen blocks the production of even that. My new doctor gave me a full thyroid panel test (along with my Vitamin D) which included checking my thyroid antibodies.
Guess what? I had Hashimotos Hypothyroid disease and low vitamin D levels. Yes, my previous doctors knew I had outgrown Juvenile Rheumatory Arthritis (another auto-immune disease) when I was younger so the increased odds of other auto-immune diseases were there. Why didn’t my first doctor wonder if I had Hashimotos Hypothyroid disease vs. just hypothyroid disease? Did you know up to 90% of all thyroid problems are autoimmune in nature—the most common of which is Hashimotos?
~~
- Let’s check your antibodies starting at an earlier certain age while we’re drawing blood for that cholesterol check we’re doing anyway. Why didn’t my first doctor check for antibodies? Or, even better, why isn’t checking for antibodies part of every physical starting earlier—before a hypothyroid diagnosis? You see often your antibodies start to rise before your TSH (the usual test for whether you are hypothyroid or not) rises into the hypothyroid range. Finding that out early gives you a chance to change your diet and lifestyle possibly avoiding the progression to Hashimotos.
By the time they diagnosed my Hashimotos, my thyroid had been under attack for over the eight years it took me to get that tested. I had no idea of the above until I began researching. It’s much more difficult to correct the damage to the thyroid after a longer amount of time—a duh.
Sadly the current fix of prescribing Synthroid® only works on balancing the hormones (T4 and T3). It does nothing to address the fact that your immune system is attacking your thyroid! Which is probably why they don’t check the antibodies early. They don’t have anything in place to address this.
I remember reading with total dismay on the Synthroid® drug fact sheet that the side effects of the drug worsen as you age and the longer you’re on the drug. So, I thought, what’s the game plan here? My step-mom’s Hashimotos had progressed to Sjögren’s syndrome—another auto-immune disease also associated with Hashimotos. I had no desire to experience what I saw her go through (loss of teeth, loss of enjoyment of food, difficulty eating due to little saliva in the mouth).
~~
- Being gluten sensitive is associated with hypothyroid disease and avoiding gluten in your diet is associated with an improvement in thyroid function. Well, that would have been excellent to know at the get-go!!
Just a couple of years prior to my thyroid diagnosis, my chiropractor (yes you heard that right) diagnosed me with gluten-sensitivity via a muscle test. My knee had swelled up and it hurt to walk, let alone go up steps. I was going up steps one at a time. An MRI showed nothing to be addressed really, save a small tear on my cartilage that “really did not need surgery”. He sent me home. I was like… “Hello?! My knee is swollen here? Do you see that? I’m not making up the pain.”
Two weeks off gluten and it was night and day, black and white difference. I wanted to kiss my chiropractor but we didn’t know each other that well. So I suspect going gluten-free helped my thyroid function for a bit longer before the TSH levels no longer measured well.
Gluten-sensitivity is associated with joint pain but so is hypothyroid disease. I personally don’t think this is a coincidence.
~~
- Hypothyroid disease is associated with high cholesterol! In fact, back in the day, high cholesterol was how they diagnosed hypothyroid disease! Right around the time I was tested for hypothyroid disease they were trying to give me diet suggestions to lower my cholesterol. You know—lower saturated fat consumption (another blog in itself), increase vegetable consumption, etc. (By the way, my HDL levels are excellent as are the triglycerides AND my cholesterol is the “fluffy” kind so even the LDL is considered acceptable.)
I had cherry tomatoes, cucumbers and peppers for lunch every day—that was it. And breakfast was a gluten free cereal with skim milk. Dinner was usually chicken with a starch and vegetable. Yes I snacked, but not excessive junk food. I prided myself on how well I ate as well as my disciplined exercise regime. If you know me, you know that I am not overweight. Giving diet suggestions was, to me, insulting. (Now my breakfasts have more protein, I eat salad daily and have less empty calories at the end of the day like chips (although they are my weakness). Dark chocolate is our dessert of choice when we indulge.) The controversy of cholesterol readings would be another blog. I just found this one in 2023 as I update this. If you follow my Better Day Yoga Facebook page, you’ll see many of my “finds”. 🙂
It is sufficient to say being told the two are related would have gone a long way toward making me feel less inadequate. Your thyroid function affects your cholesterol measures.
~~
- Being hypothyroid means I probably don’t convert Beta-Carotene to Vitamin A well. Vitamin A is important for thyroid function. Since Vitamin A is fat-soluble, you can overdose on it. It gets stored in your body vs. Beta Carotene, which is water-soluble. Typically your multiple vitamins contain Beta Carotene because healthy thyroids convert this to Vitamin A and what you don’t need is released.
Do you know how important Vitamin A is for skin health? Do you use retinols in your skin products? I’ve had cystic acne my whole life—complete with scars, tears and embarrassment at times (I know, I know—poor baby, right?).
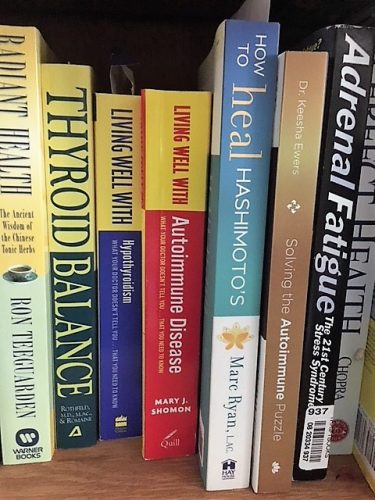
Another chiropractor I went to a few years ago suggested I take a thyroid support supplement. Once I started to take this supplement, my cystic acne went away. This was only a few years ago. I’m 57. I wanted to dance the jig when I noticed this side benefit. I noticed the supplement contained Vitamin A vs. Beta Carotene. This concerned me so I pulled out my thyroid books (of which I had way too many) and researched it some more and realized the conversion of Beta Carotene to Vitamin A doesn’t work well for people like me.
I should mention here that earlier, I had started using a Vitamin B cream on my areas of concern in lieu of clindamycin (which is an antibiotic) for my acne. I was trying to be more holistic overall. Vitamin B cream helped tremendously but the cystic acne was still occurring. I could just treat it a bit better and ward it off with the “B” cream. FYI, a sluggish thyroid can also make you deficient in certain B vitamins.
~~
- There are certain foods you might want to avoid (in addition to gluten) to manage hypothyroidism—like cruciferous vegetables (unless their cooked and you limit the amount you eat and spacing the consumption of these foods for several hours before and after your prescription medicine).They may block your thyroid’s utilization of iodine. A diet too high in fiber can alter our absorption levels of your thyroid medications. This one boggled my brain. Again, these are foods that are good for you so I don’t avoid them. I just am aware too much of a good thing can simply be too much. If you standardly consume high fiber, your blood tests will reflect that in the dosage of your thyroid medication. Talk to your doctor.
You might try an auto-immune paleo diet. It’s helped some extremely.
Some suggest avoiding night shade vegetables (potatoes, peppers, tomatoes, eggplant). Remember the lunches I was having when first diagnosed? I think the sensitivity to nightshade varies per person, as do most of these recommendations. I try not to overdo it but still consume them because I decided these foods are healthy and I refuse to avoid them all together. That’s my personal choice. You make your choice after consulting your doctor or dietician. I’ve tried avoiding them with no change in symptoms, but truth-be-told I probably didn’t avoid them long enough. My husband and I muscle test pretty much everything now though. Night shade vegetables can also affect arthritic joints.
You shouldn’t take your prescription medicine along with calcium supplements or coffee. So for most of you taking your prescription meds in the morning means waiting to have your vitamins and coffee. (I take my prescription later in the day. Some research suggests taking your prescription later in the day is more effective.)
Excess fat and sugar is never good but remember I said diabetes and hypothyroid disease are associated. So are gallbladder issues and hypothyroid disease. So breaking down fats can become an issue. Personally, I eat plenty of healthy fats like ghee, fish and coconut oils. I’d add avocado here but I’m allergic! (It’s a common allergen.) That’s my choice after my own research. You do yours and consult with your doctor!
You may want to avoid soy foods, which includes edamame, tofu, and miso. There’s some controversy on this one. Do your own research.
We should all avoid packaged foods and eat closer to nature. If it doesn’t look like it came from the earth, some would say don’t eat it. Do I follow this all the time? No. But I do for a majority of my diet. Hypothyroid disease is associated with blood pressure issues—as is eating packaged foods because of sodium content. Now I’m reading that both high and low blood pressure can be associated with thyroid disease.
Avoiding alcohol is recommended but red wine “on an occasional basis is fine for some people. Red wine is my alcohol of choice.
~~
- Flouride in your drinking water is correlated with a rise in an underactive thyroid! We are now using a reverse osmosis system and using a fluoride-free toothpaste. Did you know that fluoride was used to treat hyperthyroidism up until the 1950s?~~
- Mercury from amalgams can accumulate in your thyroid. If you’re hypersensitive to metals, this can be a problem with symptoms that overlap Hashimotos.
I’m currently in the process of switching from the standard treatment for hypothyroidism to a compounded formula. Without losing your interest, the standard treatment is giving you a hormone that is supposed to convert to another (T4 to T3) and fill the bill for both. Well, I wasn’t converting well. So they’re now working on a supplement containing T3 too. I wonder how many people are on the standard T4 and still feel lousy without checking further?
I think it might have been beneficial for a doctor to say exactly what she said as option #1. Many take this Synthroid® and they’re good to go, BUT if you want to investigate other lifestyle changes via your diet, here’s a good dietician and/or endocrinologist I’d recommend—option #2. AND by, the way, here’s some facts about hypothyroid disease that you should be aware of. So yes, your cholesterol is a bit high, but it can happen with hypothyroid disease. Here’s what we can do….
I’m still learning. I just read that some scientists are beginning to consider the possibility that Alzheimer’s disease is an auto-immune disease. My dad passed away of Alzheimer’s so believe me—I don’t want to go there! Keep on learning. I hope you found some of this useful. I just needed to download. Thanks for listening! Here’s to your health!